
by Usman Zahir, MD
Scoliosis is an abnormal curvature of the spine. Instead of going from top to bottom in a relatively straight line, a spine with scoliosis may appear to have a side-to-side “S-shaped” or “C-shaped” curve. It affects about 7 million Americans.1 Mild degrees of scoliosis do not cause any problems, but more severe cases can result in pain, weakness, and low self-esteem because of obvious cosmetic deformity. Very severe scoliosis can cause heart and lung problems if those organs are overly cramped in an abnormally shaped chest cavity.
Children may also have kyphosis, which is an abnormal forward curve, usually the upper back.
Scoliosis
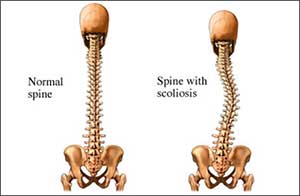
Copyright© Nucleus Medical Media, Inc.
Most cases of scoliosis begin when a child is around 8-10 years old with gradual progression of the abnormal curvature as they continue to grow. It is possible, though, for scoliosis to present at any age, including newborns.
Types of Scoliosis
There are several types and classifications of scoliosis:
Structural
Structural scoliosis is the most common form of scoliosis. It involves spinal rotation in addition to the side-to-side curvature of the spine. This type of scoliosis affects the spine’s structure and is considered permanent unless the spine receives treatment.
It results in a rotation of the spine that is typically fixed. Specific types of structural scoliosis include:
- Congenital—a rare condition that affects 1 in every 10,000 births. It occurs during fetal development and is usually present at birth.
- Syndromic/Neuromuscular—occurs as a result of an underlying health condition that affects the nerves, muscles, or bones in the back and spine.
- Idiopathic—occurs in about 8 in 10 cases of scoliosis. This type of scoliosis has no specific cause, but is likely due to a combination of genetic factors.
- Degenerative – occurs from age related changes in our spine, commonly seen in older adults.
Structural scoliosis also may be classified by age at onset as3:
- Congenital—develops between birth and age 3.
- Infantile—develops between ages 4 and 9.
- Adolescent—develops between ages 10-18.
Functional
Functional scoliosis is the result of an underlying condition that affects the alignment of the spine due to muscle imbalances, differing leg lengths, or other health conditions that cause the muscles to tense and spasm. Treating the underlying condition can reverse this type of scoliosis.
Curved Patterns of the Spine2
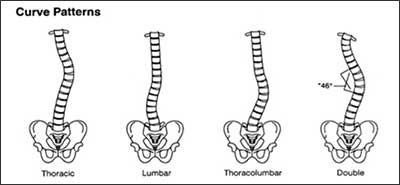
Source: National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Risk Factors
A risk factor is something that increases your likelihood of getting a disease or condition. It is possible to develop scoliosis with or without the risk factors listed below. The more risk factors you have, however, the greater your likelihood of developing scoliosis. If you have a number of risk factors, ask your doctor what you can do to reduce your risk.
Medical Conditions
A number of medical conditions predispose children to scoliosis, including:
- Turner syndrome
- Neurofibromatosis
- Muscular dystrophy
- Polio
- Cerebral palsy
- Marfan syndrome
- Friedreichs ataxia
- Rheumatoid arthritis
- Osteogenesis imperfecta
- Spina bifida
- Myelomeningocele
- Syringomyelia
Age
The adolescent form of scoliosis is by far the most common form. This form begins in children over the age of 10, and usually progresses until growth stops in adolescence.
Gender
Mild curves affect boys and girls equally, but girls are 10 times more likely to have curves that progress enough to require treatment.
Genetics
You are more likely to have scoliosis if other members of your family do. While you cannot predict how severe your scoliosis will be based on the severity of scoliosis in other family members, some evidence suggests that genetic testing might be useful in predicting the future severity of scoliosis.
Symptoms of Scoliosis
Scoliosis often is diagnosed during a routine well-child checkup or school screening. A child with scoliosis may not yet have any symptoms. More severe degrees of curvature may cause noticeable symptoms, like:
- Uneven shoulder blades.
- Uneven hip bones.
- Prominent shoulder blades or ribs on one side.
- Uneven waist.
- Appearance of leaning to one side.
- Muscle fatigue after sitting for a long time.
- Back pain.
A Woman With Scoliosis
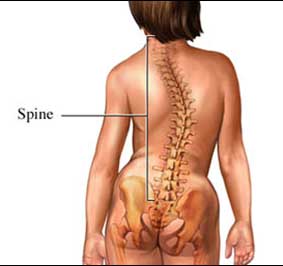
Copyright© Nucleus Medical Media, Inc.
How is scoliosis diagnosed?
Scoliosis often is initially noticed during a routine school screening or during an annual physical exam. Once scoliosis has been noted, a baseline study to measure the degree of curvature will be performed. Monitoring will be performed at regular intervals in order to keep track of the progression of scoliosis and to provide treatment if the curvature becomes more severe. Tests may include:
Forward bend test —With feet and knees together, the child is asked to bend forward with arms dangling. The screening person will stand first behind the child and then in front to check for any visible curvature, or any uneven appearance in the rib cage, hipbones, or shoulder blades.
Inclinometer or scoliometer —This device is used to measure the actual degree of curvature. The child will be asked to stand with feet and knees together, and bend forward until the examiner can see a curvature in the upper spine. The inclinometer is then placed on the back, and a measurement is taken. Another measurement is taken when the patient has leaned over further, and the area of curvature is visible in the lower spine.
Back x-rays —This is the most accurate way to diagnose and to monitor the progression of scoliosis. The x-ray can identify the presence of scoliosis, and the examiner can calculate the degree of curvature.
MRI scan — MRI scans can be used to diagnose and monitor the progression of scoliosis, but they are very expensive and no more helpful than x-rays. MRI exams are usually reserved for those who are suspected of having some other spinal condition.
Treatment
Scoliosis is monitored regularly and carefully to evaluate progression of the curvature. The treatment and management of scoliosis may involve bracing or surgery. At this time, there are no medications for the treatment of scoliosis. Typically, treatment is reserved for curvatures greater than 20°-25°, while surgery usually is recommended for curvatures greater than 40°-50°. The goals of treatment for scoliosis include:
- Stopping the progression of scoliosis.
- The possibility of lessening the curve with surgery.
- Avoidance of complications in adulthood, such as lung disease due to restriction of a deformed chest cavity.
Treatment depends on several factors, including:
- The person’s age.
- How much more he or she is likely to grow.
- The degree and pattern of the curve.
Treatment may involve observation, surgery, bracing, or casting:
- Surgery—Doctors use surgery to correct a curve, keep it from getting progressively worse when the person is still growing, or when the curve is severe. Surgery usually involves fusing together two or more bones in the spine. The doctor also may put in a metal rod or other device. These devices help keep the spine straight after surgery.
- Other treatment like braces or casting: Limiting the motion of the spine enhances the healing process of bone, and usually decreases lower back pain.3
Sources:
1National Scoliosis Foundation (NSF)
2National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)