
Total Knee Replacement, Arthroscopy, and Knee Osteotomy
Depending on the extent of the knee injury, there are three main surgical options. The least invasive is arthroscopy, which uses small incisions and specialized tools to repair the knee. The second option is knee osteotomy, which focuses on fixing one section of the knee. The third option is a total knee replacement, which replaces the entire knee joint with prosthetic components.
1. Knee Arthroscopy
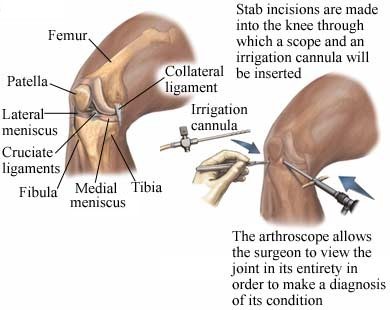
Knee arthroscopy is a surgery done to visually examine a joint. Most of the time, it is done on large joints like the knee or shoulder to help diagnose an injury or condition. Arthroscopy is performed using a special tool called an arthroscope, which is an instrument that looks like a long tube with a miniature camera on the end. Using the arthroscope and other tools, surgeons make repairs or corrections to the affected joint.
Diagnostic Arthroscopy of the Right Knee
Reasons for Knee Arthroscopy
Arthroscopy is used to see, diagnose, and treat problems inside your knee joint. The procedure is most often performed to:
- Diagnose an injury or disease inside a joint.
- Remove bone or cartilage.
- Repair tendons or ligaments.
Potential Complications
Problems from the procedure are rare, but all procedures have some risk. Your doctor will review potential problems, like:
- Infection
- Blood clots
- Swelling or bleeding
- Damage to blood vessels, nerves, or other tissue
- The need to have another surgery or more extensive surgery
Factors that may increase the risk of complications include:
- Pre-existing heart or lung condition
- Obesity
- Recent or chronic illness
- Diabetes
- Bleeding disorders
- Smoking
What to expect before, during, and after a knee arthroscopy
Prior to the Procedure
Before arthroscopy, your doctor will do one or more of the following to evaluate the joint:
- Physical exam
- X-rays
- MRI scan
In addition, prior to your surgery, you should:
- Arrange for a ride to and from the procedure.
- Do not eat or drink anything after midnight the night before the procedure.
- Use a special soap, if provided to you beforehand, the morning of the procedure.
Anesthesia will prevent pain during surgery. You will receive one of the following:
- General anesthesia—you are asleep.
- Local anesthesia—the area is numbed.
- Spinal anesthetic —a numbing medication numbs the lower back.
During the Arthroscopy Procedure
Tiny incisions are made in the skin along the joint. Special tools, including the arthroscope, are inserted through the incisions. The picture from the arthroscope shows up on a screen so that the inside of your joint can be viewed. The images help the surgeon pinpoint where to cut and repair the tissue in your joint.
When the surgery is complete, all tools are removed. The skin may be closed with stitches or clips, and the incision(s) will be covered with a dressing. Any fluid or tissue that was removed can be sent to a lab for examination.
The entire procedure usually takes less than one hour, but may be longer if repairs are done.
After the Procedure
The dressings may be removed as early as the next morning, but it takes 4-6 weeks for the joint to recover. When you return home after the procedure, your doctor will suggest a physical therapy program to help speed your recovery and to protect future joint function. Pain and discomfort after the procedure are managed with medications.
The knee needs time to heal. Supportive care includes:
- Rest—Activities may be restricted at first. Normal activities are gradually resumed.
- Ice—Ice therapy helps relieve swelling. You may be advised to use heat as you return to normal activities.
- Compression—Compression bandages provide gentle pressure to help move fluids out of the area.
- Elevation—Keeping the knee elevated helps fluids drain out or prevents fluid from building up.
- A knee brace to stabilize the knee.
- Crutches to keep extra weight off of the leg.
Contact your doctor right away if your recovery is not progressing as expected or you develop complications like:
- Signs of infection, including fever and chills.
- Redness, swelling, increasing pain, excessive bleeding, or discharge from the incision.
- Persistent nausea and/or vomiting.
- Pain that you cannot control with the medications you were given.
- Cough, shortness of breath, or chest pain.
- Joint pain, fatigue, stiffness, rash, or other new symptoms.
- Swelling, tingling, pain, or numbness in your toes that is not relieved by elevating your knee above heart level for 1 hour.
- Drainage.
If you think you have an emergency, call 911 for medical help right away.
2. Knee Osteotomy
A knee osteotomy is the removal of a wedge of bone from the tibia, also known as the shinbone, to reshape and realign the leg. Recovery time depends on certain factors, like overall health.
The Kneecap

Reasons for Knee Osteotomy
If only one section of the knee is damaged or poorly aligned, a knee osteotomy may be recommended instead of a total knee replacement. This procedure aligns the knee joint so that the healthy part of the knee surface can bear more weight. This takes pressure off the damaged part, which is often caused by osteoarthritis.
While osteotomy does not cure conditions like osteoarthritis, the surgery may:
- Reduce pain.
- Improve movement.
- Delay further damage to the joint.
- Postpone the need for total knee replacement surgery.
Possible Complications
Problems from knee osteotomy are rare, but the risk of complications may be increased if you have a history of blood clots. Your doctor will review potential problems, like:
- Infection
- Poor healing of the bone
- Excess bleeding
- Swelling
- Blood clots
- Shortening of the leg
- Injuries to nerves or blood vessels
Before your procedure, talk to your doctor about ways to manage factors that may increase your risk of complications such as:
- Smoking
- Drinking
- Chronic disease such as diabetes or obesity
- Poor nutrition
- The use of certain medications
What to expect before, during, and after a knee osteotomy procedure
Prior to the Procedure
Prior to the surgery, tests will be ordered to confirm the diagnosis and to decide how much bone to remove. Tests may include:
- Physical exam
- Blood tests
- Imaging tests:
- X-ray
- MRI scan
- CT scan
Before surgery, you will need to:
- Arrange for a ride home.
- Arrange for help at home while you recover.
- Talk to your doctor about any allergies you have.
- Ask your doctor about assisted devices you will need.
- If you are overweight, lose weight to decrease the amount of stress on your new joint.
- Install safety equipment in the bathroom, shower, and on the stairs.
- Prepare a bedroom on the first floor if possible. Climbing stairs will be difficult at first.
During the Procedure
Knee osteotomy takes about 1-3 hours. Anesthesia, including general and spinal, keeps you pain-free and comfortable during the procedure.
There are many methods that can be used to perform an osteotomy. In one method, imaging technology measures the piece of bone that will be removed. A cut is made in the skin from the kneecap to the top of the shinbone. Several thin wires are placed in the knee to serve as guides, showing where the bone should be cut. An oscillating saw removes the bone wedge. The remaining parts of the bone are held together with staples, screws, or a plate and screws. The tissue is stitched together and the area is closed.
A typical hospital stay is 2-3 days, but may be longer if any problems arise.
After the Procedure
At the Hospital-Right after the procedure, you will be taken to recovery and monitored closely. The staff may:
- Give medication to:
- Reduce pain
- Prevent infection
- Prevent blood clots
- Place padded bandages over the incision sites.
- Apply ice to reduce swelling.
- Give you a splint or brace to hold the knee in the right position.
At Home-To help ensure a smooth recovery at home, take these steps:
- Start working with a physical therapist once you are instructed to do so. The therapist will focus on balance, range-of-motion, and strength training.
- Maintain a healthy weight after surgery.
- Follow your doctor's instructions.
You will need to return to the doctor to have your cast removed or to have x-rays taken. Full recovery can take 6 months.
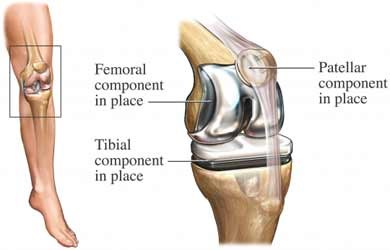
Total Knee Replacement
Knee replacement, also called arthroplasty, is a surgical procedure to replace a knee damaged by disease or injury. Recovery may take several weeks to months depending on your overall health.
Total Knee Replacement
Reasons for Total Knee Replacement
A total knee replacement may be performed if you have chronic pain and stiffness in the knee joint that limits activities. Knee replacement surgery is most often done to:
- Ease knee pain and disability due to arthritis or previous severe knee injury.
- Correct a knee deformity.
Potential Complications
Complications from knee replacement surgery are rare, but all procedures have some risk. Your doctor will review potential problems, like:
- Infection
- Excess bleeding
- Swelling
- Blood clots
- Chronic weakness in knee joint
- Worsening or unchanged pain
Factors that may increase the risk of complications include:
- Smoking
- Poor nutrition
- History of blood clots
- Long-term illness
- Use of certain medications
What to expect before, during, and after knee replacement surgery
Prior to the Procedure
Your doctor will likely do the following:
- Physical exam
- Blood tests
- X-ray
- MRI scan to get images of the internal structure of the knee
Before surgery, you will need to:
- Arrange for a ride home.
- Arrange for help at home while you recover.
- Talk to your doctor about any allergies you have.
- Ask your doctor about assist devices you will need.
- If you are overweight, lose weight. This will help to decrease the amount of stress on your new joint.
- Install safety equipment in the bathroom, shower, and on the stairs.
- Prepare a bedroom on the first floor if possible. Climbing stairs will be difficult at first.
Talk to your doctor about any medications, herbs, or supplements you take. You may be asked to stop taking some medications up to 1 week before the procedure. Do not eat or drink anything after midnight the day before your surgery, unless told otherwise by your doctor.
During the Knee Replacement Surgery
Knee replacement surgery is done in a hospital setting, and typically lasts about two hours. The normal length of stay in the hospital is 3-4 days, but may be longer if complications arise.
Anesthesia keeps you pain-free and comfortable during the procedure. General anesthesia keeps you asleep during the procedure. Regional anesthesia numbs the lower part of the body.
A cut is made in your skin, and the damaged cartilage and bone is removed. The remaining bone is prepared to receive the new joint made from materials like plastic and metal. The artificial joint is placed in the proper position, and may be cemented within the bone. The incision is closed with staples and a drain is left in to allow extra fluid to flow out.
After the Procedure
At the Hospital:
Right after the procedure, you will be taken to recovery and monitored closely. The staff may give you:
- Pain medication
- Antibiotics to prevent infection
- Medication that prevents blood clots
While recovering at the hospital, you may need to use a continuous passive motion machine, which is designed to:
- Slowly move your knee
- Restore function
- Decrease swelling
- Improve circulation
During your recovery, you will need to:
- Move your foot and ankle to increase blood flow back to your heart.
- Wear support stockings. These may help prevent blood clots from forming in your legs.
- Work with a physical therapist, which may start as soon as the day after surgery. You will learn safe ways to move your knee and support your weight.
- You will learn how to use a walker, crutches, or other support devices.
At Home: To help ensure a smooth recovery at home, take these steps:
- Start working with a physical therapist once you are instructed to do so. The therapist will focus on balance, range-of-motion, and strength training.
- Maintain a healthy weight after surgery.
Within 6 weeks, you should be able to go back to light activities and driving. You may feel a soft clicking in the joint when walking or bending. Continue to work with the physical therapist. Water-based exercises can help to improve joint pain, swelling around the knee, and range of motion.
Note that antibiotics may be needed before certain dental procedures or surgeries now that you have an artificial joint. This will prevent possible infections from entering the bloodstream. Make sure to let the dentist or doctor know that you have an artificial joint.
Sources:
American Orthopaedic Society for Sports Medicine
Arthritis Foundation
Ortho Info—American Academy of Orthopaedic Surgeons