
by Courtney Subudhi, CNM, Virginia Complete Care for Women
A certified nurse-midwife (CNM) is a registered nurse who has earned a graduate degree in midwifery, which trains him or her to handle normal, low-risk pregnancies and deliveries, care of the infant up to 28 days of life, and gynecological care.
In the United States, the first nurse-midwifery program dates back to 1932. CNM programs are certified through the American College of Nurse Midwives and their board certification is done through the American Midwifery Certification Board (AMBC)1, or the North American Registry of Midwives (NARM)2. These are both national organizations that maintain the same requirements for professional practice standards in each state. Only graduates of accredited programs are eligible to take the nurse-midwifery certification exam. CNMs are licensed at the state level but they are eligible for licensing in all 50 states.
Types of Midwives
While there are different types of midwives with varying degrees of education, CNMs are recognized as the most highly trained and skilled. The different types of midwives and their educational requirements are3:
- Certified Nurse-Midwife (CNM): a midwife trained and licensed in nursing and midwifery. Nurse-midwives must have at least a bachelor’s degree from an accredited institution. They also take a national board exam and are board certified by the American Midwifery Certification Board (AMBC). The midwives you see at Virginia Complete Care for Women at CNMs.
- Certified Midwife (CM): an individual trained and certified in midwifery. Certified midwives must have at least a bachelor’s degree from an accredited institution, but this does not have to be in nursing. They are also certified by the American Midwifery Certification Board (AMBC). CMs are not able to be licensed in all states. They are able to practice in New York, New Jersey, Rhode Island, Delaware, Maine and Missouri.
- Certified Professional Midwife (CPM): an individual who is trained in midwifery and meets standards of the North American Registry of Midwives. Multiple educational backgrounds are recognized to become a CPM.
- Direct-Entry Midwife (DEM): an independent individual trained in midwifery through various sources that may include apprenticeship, self-study, a midwifery school, or a college/university program. They are licensed and regulated in 21 states.
- Lay Midwife: an individual who is not certified or licensed as a midwife but has received informal training through self-study or apprenticeship. They are licensed and regulated in 21 states.
What kind of care does a midwife provide?
Midwives provide continuous care for women with uncomplicated pregnancies throughout their pregnancy term, labor, delivery, and postpartum care. In addition, a midwife may provide gynecological care, routine annual exams, pap smears, contraceptive counseling, prescriptions, and ongoing care of the mother after the birth of her baby. Midwives usually do not work with high-risk pregnancies or women with chronic diseases, but often work closely with a physician who is available for collaboration, consultation or to assume care if complications arise. A CNM’s comprehensive model of care may include4:
- Monitoring the physical, psychological, and social wellbeing of the mother throughout her childbearing cycle.
- Providing the mother with individualized education, counseling, and prenatal care, continuous hands-on assistance during labor and delivery, and postpartum support.
- Minimizing technological interventions.
- Identifying and referring women who require obstetrical attention.
A CNM focuses on eliminating unnecessary procedures, takes a more holistic approach to the overall health of a woman, and typically relies less on medical tests and devices than traditional medicine. This, in turn, can create a more natural, intimate experience for a pregnant woman and her family. A CNM can, however, order diagnostic tests, labs, and perform procedures if necessary based on the patients’ needs.
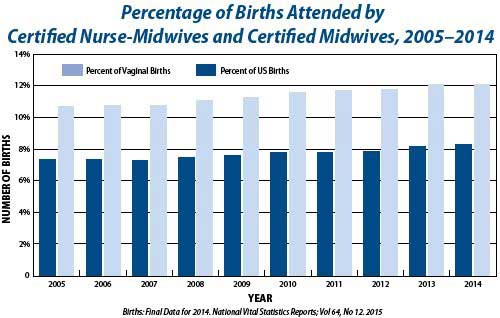
CNMs have improved the level of care for many women, particularly those in rural or inner-city populations by increasing access to and providing quality health care. Choosing to use a midwife for delivery is at an all-time high in the United States. Many CNMs have payment plans and accept most insurance plans, including Medicaid. There is no additional cost to seeing a CNM. However, with the attention on high touch, low-tech care, many women save health care dollars due to unnecessary medical procedures.
Where do CNMs deliver babies?
Certified nurse midwives deliver babies in:
- Hospitals - In the U.S., about 90% of midwife-attended births take place in a hospital setting.
- Birthing Centers - A birthing center is a healthcare facility that can be staffed by CNMs, or CPMs with an obstetrician available in case of emergency. The midwife will usually have an agreement with an MD for transfers. A birthing center provides a more home-like setting than a hospital and accounts for about 3% of U.S births that have an attending midwife.
- Home - Some low risk women may choose the comfort of home for low-risk births. These women would be transported to the hospital for an emergency if needed. Fewer than 3% of U.S. births take place at home with a midwife.
Is delivering with a midwife as safe as delivering with a doctor?
The Cochrane Library5, a collection of independent evidence to help inform healthcare decision-making, conducted a review of several past studies to determine the safety of midwife birth when compared to traditional hospital delivery. The review included 11 trials with more than 12,000 women who used a midwife. They found that there was no increased risk of infant death over a traditional hospital delivery and, in fact, women who gave birth with midwives had many benefits4, including:
- Decreased risk of needing a C-section.
- Reduced rates of labor induction and augmentation.
- Reduced use of regional anesthesia.
- Decreased infant mortality rates.
- Decreased risk of preterm birth.
- Decreased third and fourth degree perineal tears.
- Decreased need for forceps or vacuum-assisted births.
- Lower costs for both clients and insurers.
- Increased chances of having a positive start to breastfeeding.
- Shorter hospital stays for infants.
- Increased satisfaction with quality of care.
How Does This Affect You?
One of the most positive impacts of a rise in midwife-assisted births is that it helps give women and their partners a choice in how their child comes into the world as well as increases positive outcomes on maternal and neonatal mortality and morbidity. There are many different birth programs and options, so look for a program that make you feel the most comfortable. Whatever your choice, whether you choose an obstetrician/gynecologist, more personalized midwife-assisted delivery, communicate your birth plan preferences to the provider you choose. Remember that there are varying levels of training among midwives, so make sure to discuss these when searching for one. If you have a high-risk pregnancy or other chronic illness, you should discuss your options with your doctor or midwife to see if midwifery care is right for you and your family.
Primary Sources:
1American Midwifery Certification Board
2American College of Nurse-Midwives (ACNM)
3North American Registry of Midwives (NARM)
4American Pregnancy Association
5The Cochrane Library
Other Sources:
Centers for Disease Control and Prevention (CDC)
Bureau of Labor Statistics